Insurance Exam Vocabulary Terms
Preferred Provider Organization (PPO)
arrangement, insured or uninsured, where contracts are established by Health Plan Companies (typically, commercial insurers, and, in some circumstances, by self-insured employers) with health care providers. The Health Plans involved will often designate these contracted providers as "preferred" and will provide an incentive, usually in the form of lower deductibles or co-payments, to encourage covered individuals to use these providers. Members are allowed benefits for non-participating provider services on an indemnity basis with significant copayments and providers are often, but not always, paid on a discounted fee for service basis.
Other terms you may be interested in:
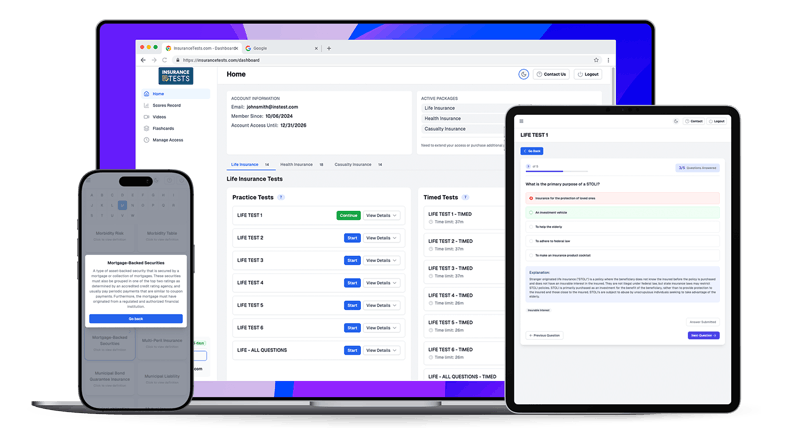
Our Insurance Exam Prep Includes...
- Hundreds of Insurance Practice Test Questions (that apply to your state)
- Insurance Vocabulary Flashcards
- Study-Mode & Timed-Exam Mode
- 2025 Updated Material
- User-Friendly On All Devices
- 1 Week / 1 Month / 3 Month Access
- Insurance Exam Tip Videos
- Support From Licensed Instructor
- Insurance Terms & Glossary
- 100% Pass Money-Back Guarantee★